When we talk about infection prevention and control (IPC), people assume things like personal protective equipment (PPE) or perhaps hand hygiene. People perceive that it’s about reacting when there is an outbreak to stop an infectious disease – they picture hazmat suits and shipping in of essential resources, often on a temporary basis to deal with the immediate crisis at hand.
An example of a high profile IPC focus is World Hand Hygiene Day (WHHD), commemorated every year on 5 May, and bringing people together to maintain the profile of this life saving action. There is nothing wrong with this as a springboard for engagement and action on IPC. It is nothing more or less than a way to engage and stimulate action – both short-and long-term. But just as with this year’s WHHD slogan, it might be 5 May, or an outbreak, but hand hygiene and other IPC interventions are always needed at the right moments.
Nobody puts IPC in the corner!
Let’s look at the bigger picture of IPC.
To a person accessing health care (and their families/loved one), IPC is or should be a contract that guarantees their safety from the harm of health care associated infections (HAI) through the delivery of evidence-based care, given that HAIs are amongst the most frequent adverse events;
To a health care worker providing care, IPC is or should be the way they practice every day – their norm – delivering evidence based safe, compassionate care;
To a healthcare manager, IPC is or should be a flagship specialist service, staffed adequately and supported to assure the organisation and all who enter it that all of the elements that are needed to be in place to keep health workers and patients safe are in place;
To a politician IPC should be a central part of health care policy, mandated and legislated so that across the entire health system it is embedded in policies, procedures and practices.
As such, IPC is something that needs to be both built and seen intentionally, with foresight.
In results from a recent online poll, respondents from a number of countries saw IPC as having breadth beyond the usual assumptions and perceptions and outlined IPC activities as having the potential to influence health and well-being, alongside safe water sources and sanitation for all. Probably not surprising, but people also said IPC was relevant to things like partnerships in the context of achieving the sustainable development goals (SDGs). People also stated that IPC action could achieve political commitment, and as such a healthcare safety culture and the necessary behaviour change.
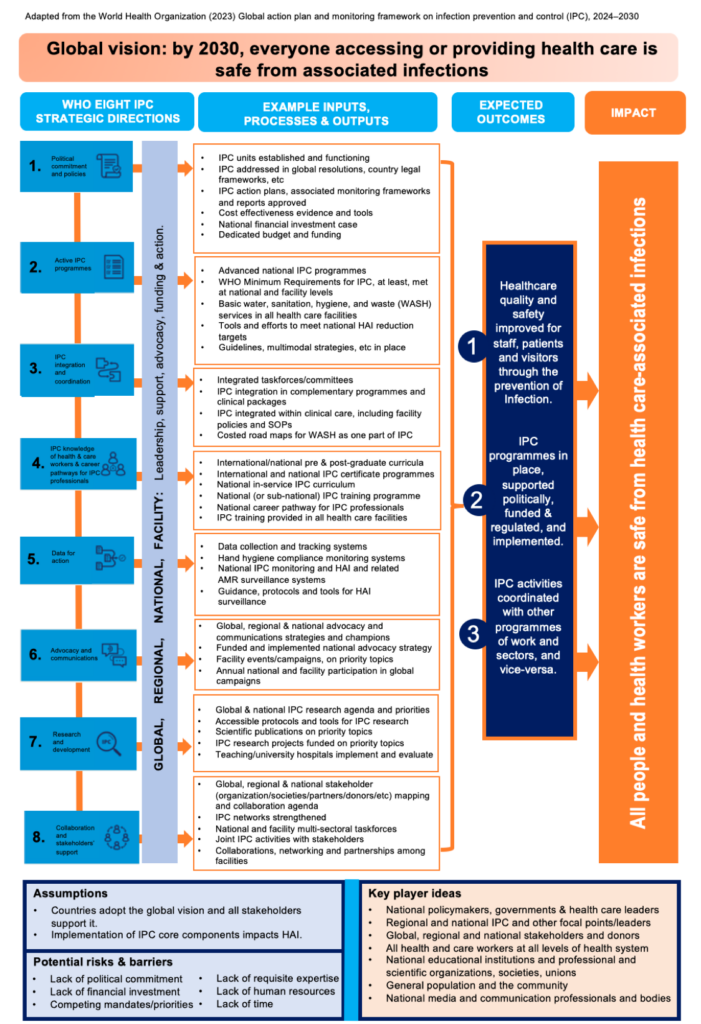
If politicians and health care managers perceive IPC as only really about PPE and outbreak responses, we have a problem. Shifting thinking on the value that IPC brings to societies and all peoples requires leadership. Many leaders in many countries are showing leadership in this regard and they’re being supported by a global vision and a global IPC strategy. Turning these into a long-term, sustainable action plans in every country, today, tomorrow, on 5 May, quite soon, is needed in order to get on top of the very real, every day problem of HAI. In fact, this is perhaps as urgent as the need for life-saving resources provided during outbreak situations.
Creating a sense of urgency around every-day IPC is therefore key. As well as national leadership, this is part of IPC management and leadership in every health care facility of the world. Strengthening IP competence in this area, alongside the many other management, leadership and biomedical skills is a fundamental necessity.
And all because an increase in HAI cases and the frequency of outbreaks will be affected by no clear IPC strategy or long-term implementation plan. We are just finishing the writing and design of a new guide to implementation for IPC national action plans – to be launched by the World Health Organization in June. And:
- While, 30% of countries do not have an active national IPC programme (that is, a functioning programme with an annual workplan and budget) there remains a risk.
- With only 38% (57 of 150) of countries having a national IPC curriculum, gaps remain, which require leadership and a sense of urgency across the world.
Some resources do exist to enhance, for example, IPC guidelines, IPC training and education packages, etc. But there is more to do. This is what we can achieve with strategies, planning and effective implementation:
Do you want to update your plans, implement more efficiently, and increase your impact? This is your chance! Let’s not just see outbreaks as the thing we need to react to urgently. Let’s not just see hand hygiene and IPC action as being important only during outbreaks or on global days/internationally appointed weeks…
Together, we can better:
- Strategise and plan
- Give the right policy advice
- Find out the current situation through insightful interviews and discussions
- Write impactful reports and briefs to get attention
- Effectively implement guidance
- Provide and use effective tools
- Facilitate effective teamwork for safe practices
- Undertake effective training and education.
Talk to us about using our insights and resource templates, and about building your capacity towards the vision of 2030.